Hint: Abnormal versus insufficient cells mean different diagnosis codes.
 When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.
When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.
Question 1: When a patient comes in for a second Pap smear, what CPT code(s) should you apply and why?
Question 2: Will you receive reimbursement for handling the repeat Pap smear? Why or why not?
Question 3: If the patient comes back in for a Pap smear due to abnormal results, what ICD-9 code(s) should you use and why?
Question 4: If the patient has a repeat Pap because the lab did not have enough cells in the specimen to interpret the results, what ICD-9 code(s) should you use and why?
Answer 1: Here’s What CPT Codes
When the patient comes in for a second Pap smear, submit the appropriate E/M office visit code (99211-99215). You will probably be able to report 99212 (Office or other outpatient visit for the evaluation and management of an established patient …) for this visit becausethe patient likely will come in only for the Pap smear and CPT does not include a specific code for taking the Pap. Code 99212 carries 1.08 relative value units (RVUs), unadjusted for geography. That translates to about $31 for this visit (using the new conversion factor of 28.3868).
Answer 2: Handling the Specimen Depends on Payer
Some private payers will reimburse for handling the repeat Pap smear specimen (99000, Handling and/or conveyance of specimen for transfer from the physician’s office to a laboratory). But Medicare carriers consider the collection and handling part of a problem E/M service, and you should not code for it separately.
In addition, Medicare will not reimburse for Q0091 (Screening Papanicolaou smear; obtaining, preparing, and conveyance of cervical or vaginal smear to laboratory) for the repeat Pap smear because it is a diagnostic test. In this case, Medicare considers the service a problem E/M, not a preventive screening, and the specimen collection is part of the E/M service.
Answer 3: Use 795.0X for Abnormal Results
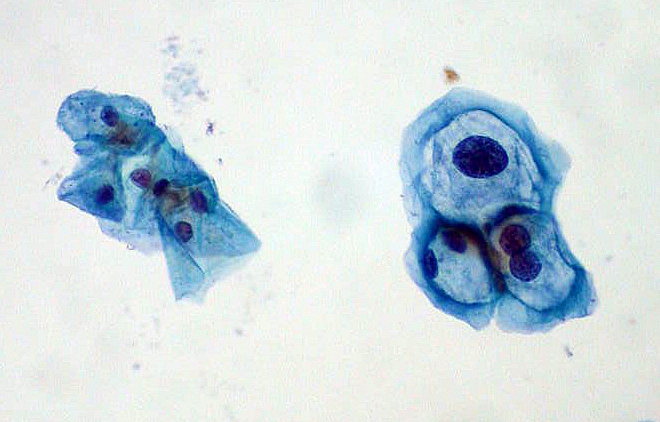
You should report 795.0x (Abnormal Papanicolaou smear of cervix and cervical HPV) if the ob-gyn repeats the Pap smear due to abnormal results.This code requires a fifth digit, points out Peggy Stilley, CPC, COBGC, ACS-OB, director of auditing services at the American Academy of Professional Coders. If you don’t include the fifth digit, this “could be a reason for a denial,” she adds.
For example, a 35-year-old woman with multiple sexual partners presents for an annual exam. She has not had a Pap smear in four years. The Pap results return ASC-US, and the physician asks her to come back in three months for a repeat Pap to follow any abnormal cell progress. When the patient returns, you should code the appropriate E/M office visit with 795.01 because the Pap is repeated due to abnormal cells.
Answer 4: ‘Inadequate Sample’ Means a Different Code
On the other hand, if the patient requires a second Pap smear because the first sample was inadequate (that is, the lab did not have enough cells in the specimen to interpret the results), you can use one of two codes. Report V76.2 (Special screening for malignant neoplasms; cervix) or 795.08 (Unsatisfactory cervical cytology smear) if the first smear was inadequate, says Karen O’Malley, office manager of an ob-gyn practice in Arlington Heights, Ill.
In the notes associated with 795.08, the ICD-9 manual indicates you can use this code for “unsatisfactory smear.” For example, the patient is menopausal and the physician does not reach the transformation zone. The Pap result indicates only a few cells (not enough to analyze), and the physician likely would require another Pap. The physician may consider this as just a second screening Pap smear, or may decide to report the available code for an unsatisfactory smear instead. Medicare would require V76.2 as the code for this situation.
ICD-10: You’ll have to use new codes when your diagnosis system changes in 2013. They are:
- 616.10=N76.0 (Acute vaginitis) or N76.1 (Subacute and chronic vaginitis),
- 795.0x=R87.61x (Abnormal cytological findings in specimens from cervix uteri),
- V76.2=Z12.4 (Encounter for screening for malignant neoplasm of cervix), and
- 795.08= R87.615 (Unsatisfactory cytologic smear of cervix).
Take more coding challenges in Ob-Gyn Coding Alert.
By: Suzanne Leder, M.Phil., CPC, COBGC, executive editor of Ob-Gyn Coding Alert, 2010; Volume 13, Number 6.
