 Here are the pros and cons to help guide your decision.
Here are the pros and cons to help guide your decision.
Question: Our practice is considering accepting patients with PFFS plans. We’re heard that some patients are starting to have them, but we’re not sure whether we’re going to accept them or not. Are PFFS plans beneficial for us?
Answer: PFFS are Private Fee-for-Service plans, which are non-network plans. These plans let members receive care from any doctor or hospital that accepts the plan’s payment terms and conditions.
If your practice decides to accept these terms, you would become a “deemed” provider. Plan members can receive covered services from any deemed provider in the U.S. However, member patients must confirm that the provider is deemed every time a service is provided.
PFFS plans are different from Medicare Advantage plans because they do not require a doctor or hospital to contract with a health plan to provide services. This means that doctors or hospitals that do not agree to the PFFS plans’ terms and conditions may choose not to provide health care services to a plan member, except in emergencies.
Coming soon: Starting in 2011, PFFS plans will have to measure and report on their providers’ quality of care. But the catch is that they’ll also have to form provider networks with contracts.
In counties where there are two or more non-PFFS plans, PFFS plans will no longer be able to simply “deem” providers into the plan without a contract. Under current law, PFFS plans don’t have to prove they can meet access standards if they allow any willing qualified Medicare provider to participate, and they pay as traditional Medicare would pay.
One argument is that the network requirement would provide better access to care because there would be contracts between the providers of services and the plan. On the…

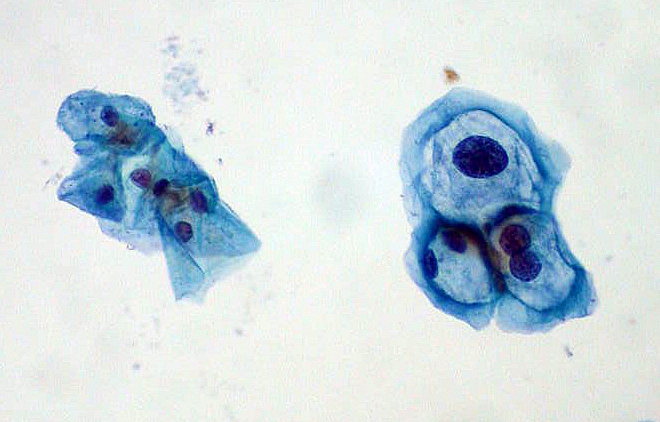 When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.
When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.